- Share this item with your network:
- Download
Pulse
- Editor's letterImproved patient outcomes underscore convergence efforts
- Cover storyPayer-provider partnerships spurred by data, value-based care
- InfographicPayer-provider partnerships may fuel future affordable care
- FeatureHospitals battle duplicate medical records with technology
- ColumnMarch to value-based healthcare results in 'payviders'
- ColumnAI technology in healthcare advances surgical, clinical support
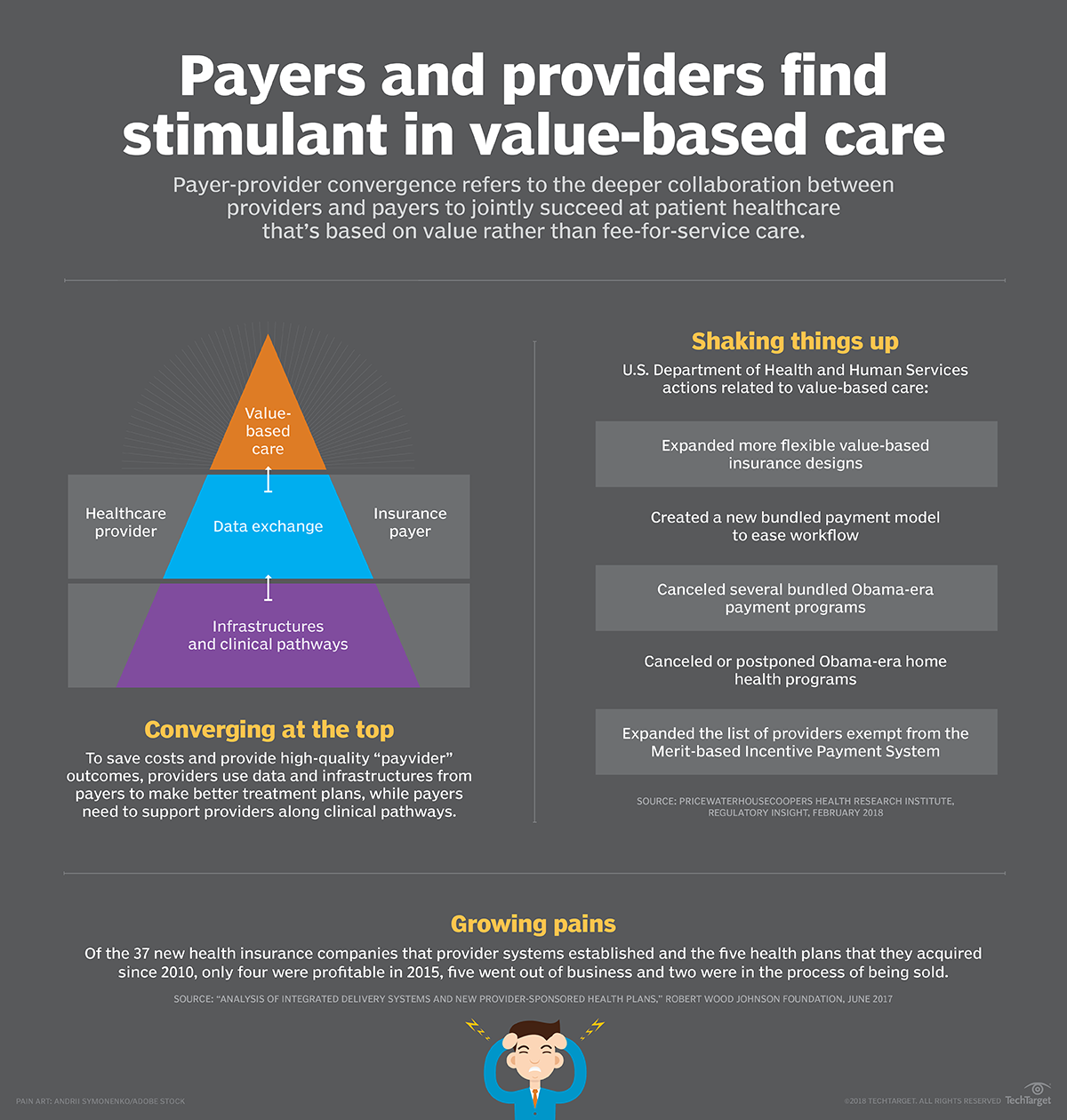
Payer-provider partnerships may fuel future affordable care
Taking an untraditional route to value-based care, payer-and-provider partnerships highlight the collaborations between benefit planners and healthcare systems.Fueled by the push to value-based care and population health management, payer-provider partnerships -- untraditional collaborations between healthcare providers and health benefit planners -- are gaining momentum.
Instead of payers independently bearing most of the patient-care risks, some providers are now encouraged to collaborate with payers throughout treatment plans, creating a win-win situation that achieves quality-based care and meets Affordable Care Act requirements. For example, under the risk-sharing model, there ideally is less runaround between providers and insurance carriers when a patient is admitted to a hospital.
The gist of the convergence is sharing and analyzing data based on the existing operations and technology infrastructures on the payer's end. Effective communication between the two parties also plays an essential role in making the partnership sustainable.
The path forward for payer-provider partnerships is not clear-cut financially based on recent evidence. For example, since 2010, 37 provider-sponsored health plans have been established, but only four were profitable in 2015, according to a report released last year by the Robert Wood Johnson Foundation.